Health Equity: Overview of Health Systems and Patient Pathway
Unequal healthcare access among different groups leads to less preventative care, and more urgent and intensive procedures. Such disparities in access currently cost the US healthcare system approximately $320 B annually and is projected to grow to as much as $1 trillion annually in 2040[1]. In economically and socially disadvantaged communities, patients face barriers that impact their ability to receive necessary and equal care.
For life sciences companies, inequities lead to patients receiving inadequate or delayed care, and in its worst form, causes patients to miss treatment opportunities that utilize their products.
Life science companies can begin to tackle some of the drivers and determinants of health equity by using a patient-centric approach, as patients’ primary point of interaction with the healthcare system is through their providers. A closer examination of those interactions can reveal how manufacturers and medical technology companies can create initiatives to support greater equity. Examining the patient pathway can reveal specific moments when inequities “add-up” causing significant treatment drop out.
Solutions to equity barriers are not static – companies need to set themselves on a continuous path to improvement. The place to start is understanding what drives friction between patients and their own healthcare and focusing on the patient-provider interaction to identify solutions and expand their presence in underserved markets.
Barriers Arise During Patient-Provider Interactions
In order to maximize patient access and health outcomes for life science companies and manufacturers, the patient-provider interaction is key to understanding barriers to treatment. Acute analysis of these barriers is the first step to understanding where life science teams have the most influence on health equity and patient treatment access.
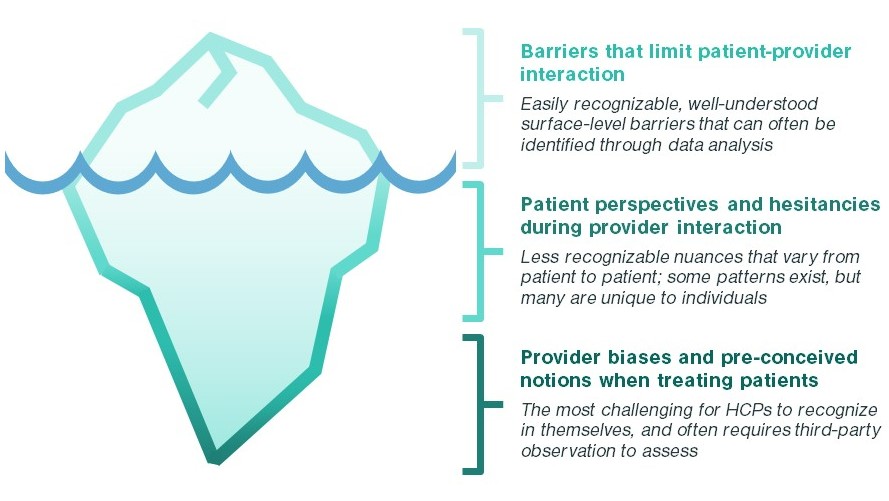
- Barriers limiting patient-provider interaction Before a patient walks into a doctor’s office, they may already face structural and socio-economic challenges impacting their interaction with the physician and their ability to follow a treatment plan. Such barriers include a lack of insurance, lack of transportation resources, and lack of availability. For example, Black Americans were 3x more likely to report loss of health insurance during the pandemic compared to white respondents. Structural and socioeconomic challenges also drive additional comorbidities, such as obesity and hypertension[2], which may limit treatment options.
- Patient perspectives and hesitancies during provider interaction When treating patients, providers interact with patient groups with differing attitudes towards the healthcare system, their diagnoses, and treatment options. For example, Black patients are more likely to mistrust the healthcare system due to long-standing racial inequalities. A nationwide poll by The Undefeated and the Kaiser Family Foundation found 7 out of 10 Black Americans say they’re treated unfairly by the healthcare system and 55% percent say they distrust it[3]. Lower trust among patients can lead to slower and less vigilant follow-up, and potentially patient drop-off from treatment. Patient groups also have varying awareness and understanding of their diagnosis due to education levels, and a patient’s perspective on the severity of a disease can be a major driver for urgency and vigilance with treatment follow-up
- Provider biases and pre-conceived notions Finally, physicians can also be impacted by racial bias, impacting the delivery of healthcare to racial minorities. Studies testing implicit association among physicians have found low to moderate levels of bias against racial minorities[4], and a public health study found 32% of Black Americans have reported being discriminated against when receiving healthcare treatment[5]. Although this bias may be unintentional, implicit bias from physicians negatively impacts patient behavior. A Journal of Family Practice study found patients who felt racial discrimination in a healthcare setting were less likely to follow physician recommendations and more likely to delay care[6]. Although many healthcare curriculums have developed to increase understanding of race-based impacts, negative impacts of bias on patient outcomes remain.
How can Kx Support Your Health Equity initiatives?
Research in Health Equity can be challenging. Understanding how to create a more equitable environment, and how to support underserved populations requires a nuanced and detailed approach to research supporting such initiatives. Kx Advisors helps clients frame research challenges using the patient pathway to understand where and how health equity initiatives should be targeted. To learn more about how Kx can support your Health Equity initiatives, contact Evelyn Tee at evelyn.tee@kxadvisors.com to learn more.
[1] McKinsey COVID-19 Consumer Survey as of June 8, 2020
[2] Akil L, Ahmad HA. Effects of socioeconomic factors on obesity rates in four southern states and Colorado. Ethn Dis. 2011;21(1):58-62.
[3] Common Wealth Fund: Medical mistrusts among Black Americans
[4] Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20(3):896-913. doi:10.1353/hpu.0.0185
[5] NPR/Robert Wood Johnson Foundation/Harvard T.H. Chan School of Public Health, “Discrimination in America: Experiences and views of African Americans,” 2017, Figure 1.
[6] Blanchard J, Lurie N. R-E-S-P-E-C-T: patient reports of disrespect in the healthcare setting and its impact on care. J Fam Pract. 2004;53(9):721–30.